For educational purposes only. Please see section 3.3 of our EULA.
User Question/Comment:
This case was submitted anonymously. It is lightly edited for clarity and formatting.
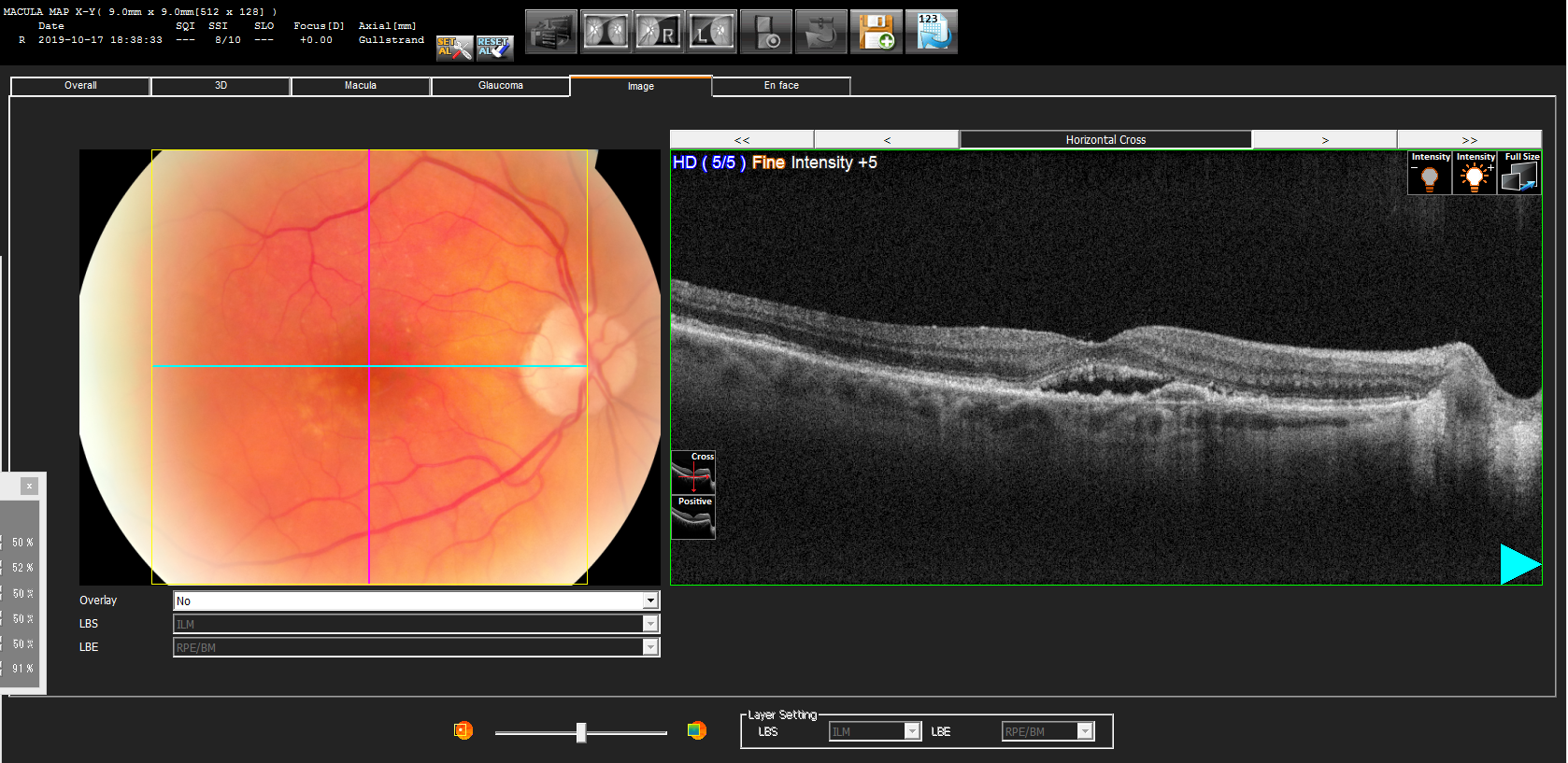
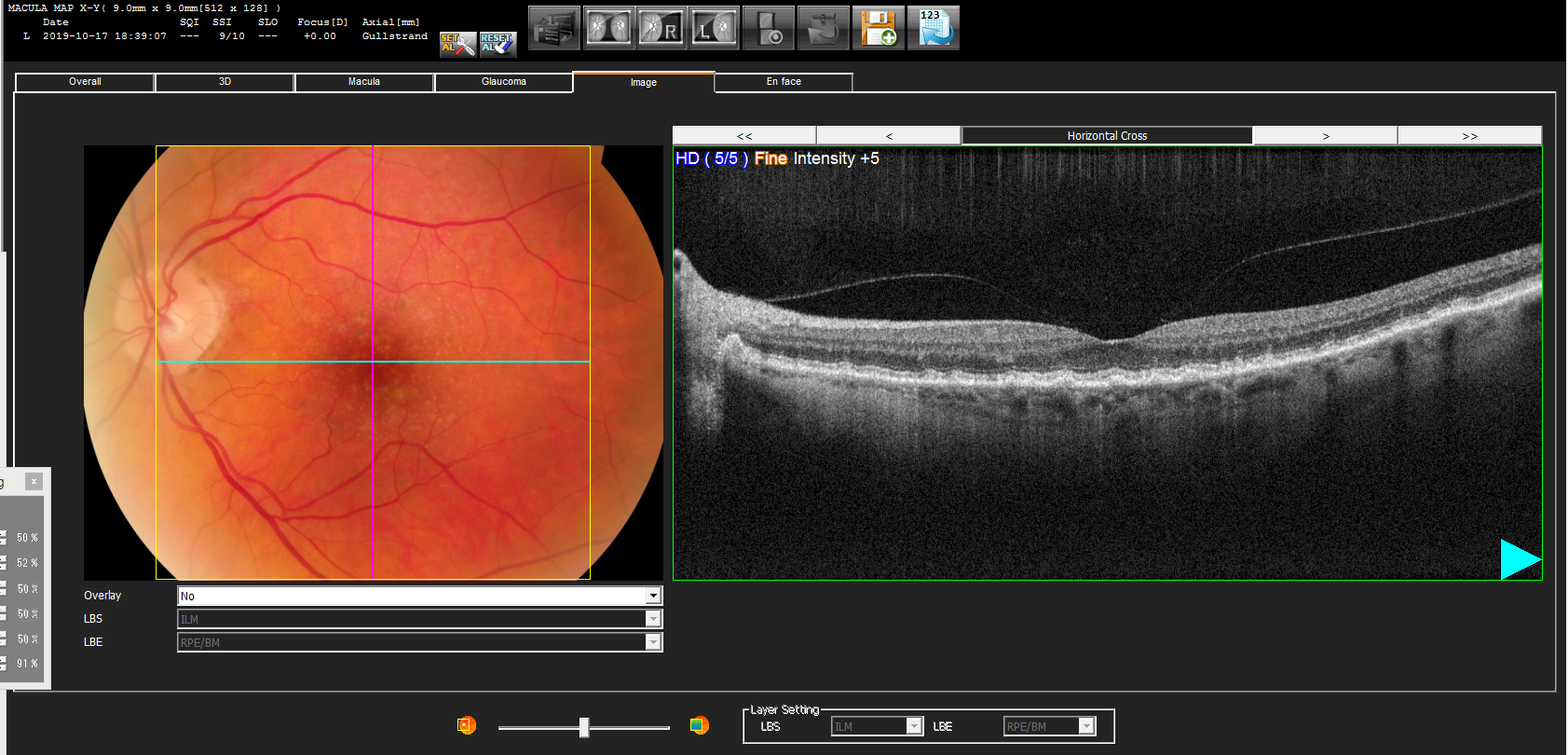
This is an 81 year-old female patient with AMD. Her VA is correctable to OD 20/40 and OS 20/25. On OCT she has subretinal fluid in her right eye. She has seen 2 retinal specialist with varying opinions. The first said she does not have CNV and no treatment is required at this time. The other says she has Wet AMD and to start injections to “sort out if this is a CNV”. Why the variable opinions?
Dr Lederer’s Response:
Very challenging question! The heart of the matter surrounds the concept of serous fluid versus exudative fluid. Let’s break it down.
Choroidal neovascular pathologies that cause abnormal blood vessels to grow and leak are termed CNV. These are responsive to anti-VEGF injections. This is because the underlying vascular tree is being driven to grow by VEGF. These vessels are of course abnormal and leak fluid. Hence, in cases of AMD, we call this Wet AMD or Exudative AMD or Neovascular AMD.
But there are also pathologies related to serous accumulation in the subretinal space due to varying other etiologies (no CNV). Think CSR (central serous retinopathy) as an example. While competing etiologic theories exist (example: too much leak from the choroid vs weakened RPE pump, etc) we know that run-of-the-mill CSR does not respond to anti-VEGF injection. This is because there is no VEGF inciting the pathology and the fluid is now termed “serous”. While this patient has drusen consistent with AMD there can still be a serous component to their disease.
So let’s go back to the case. It all comes down to imaging. Does the fluorescein angiogram show a CNV pattern or a serous pattern? Does the OCT-Angiography show CNV? Do the other OCT cuts demonstrate subretinal hyperreflective material (SHM)? Clinically, is the patient progressively worsening? Is there blood developing?
Sometimes the retinal specialist can be sure of the diagnosis based on a conglomeration of the findings. And sometimes it is just hard to know for certain. Thus different doctors will use different algorithms. For example, if you do an injection and the fluid resolves you can be pretty sure it was a VEGF-mediated process. Or perhaps you decide to observe and the next time things are worse with blood and SHM; This too would be indicative of CNV. Some cases just do not fit into a perfect box.