For educational purposes only. Please see section 3.3 of our EULA.
User Question/Comment:
This case was submitted by Dr Mona Sandhu. It is lightly edited for space and formatting.
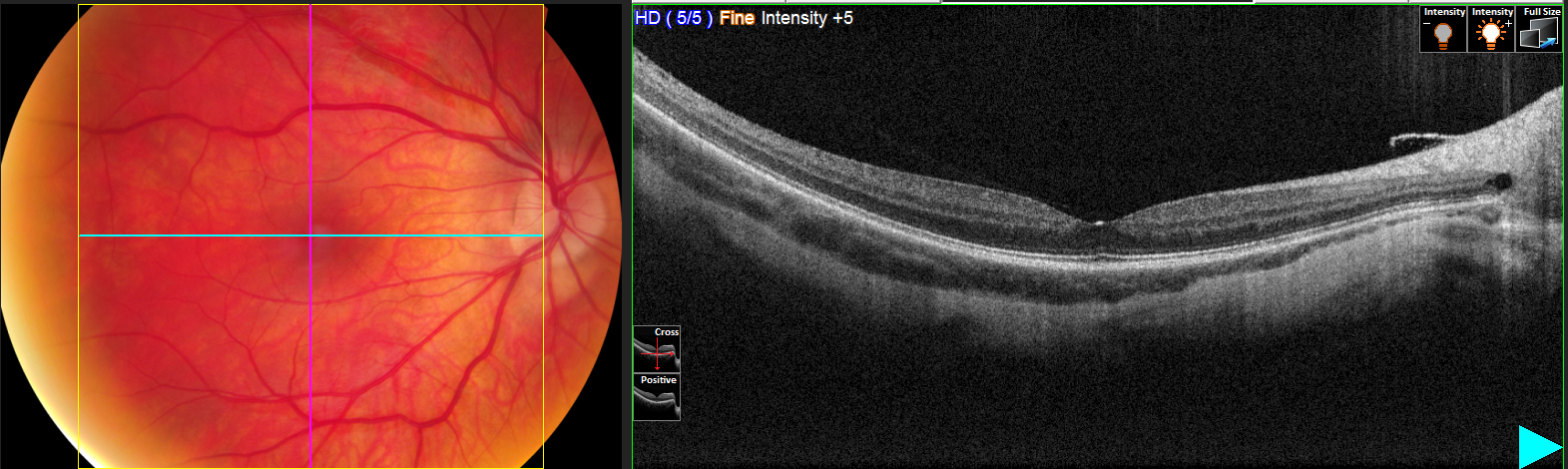
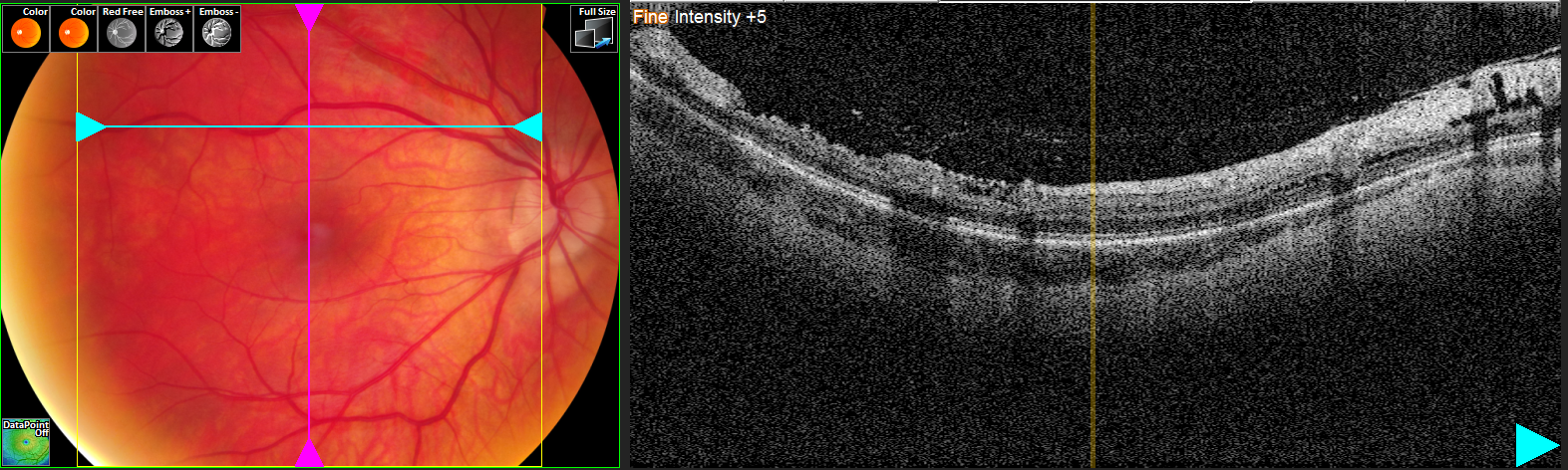
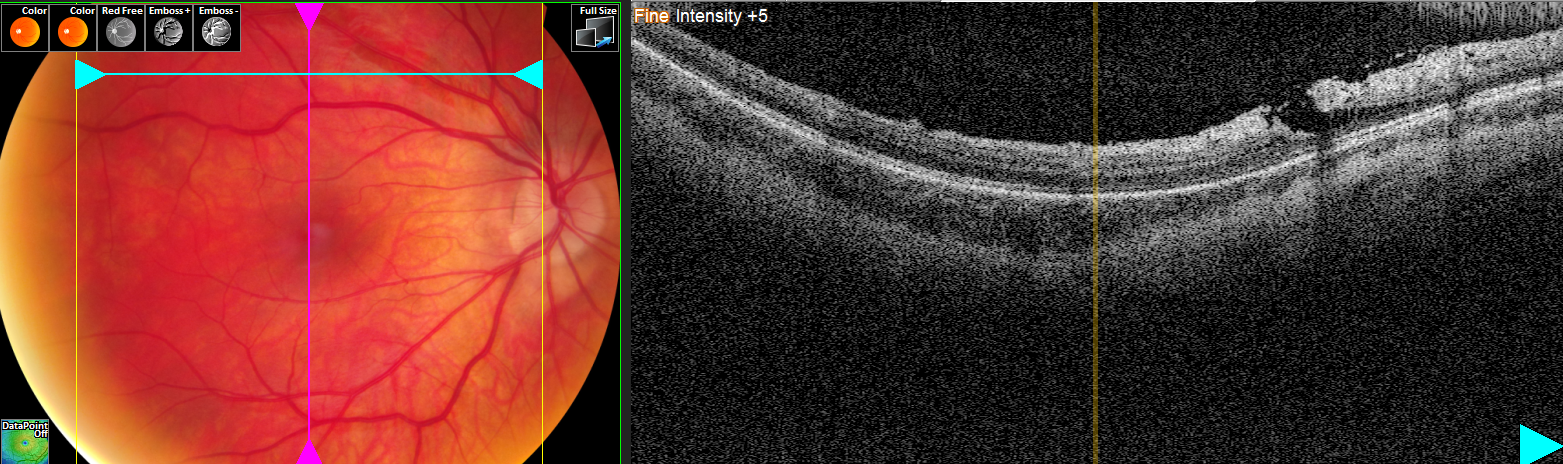
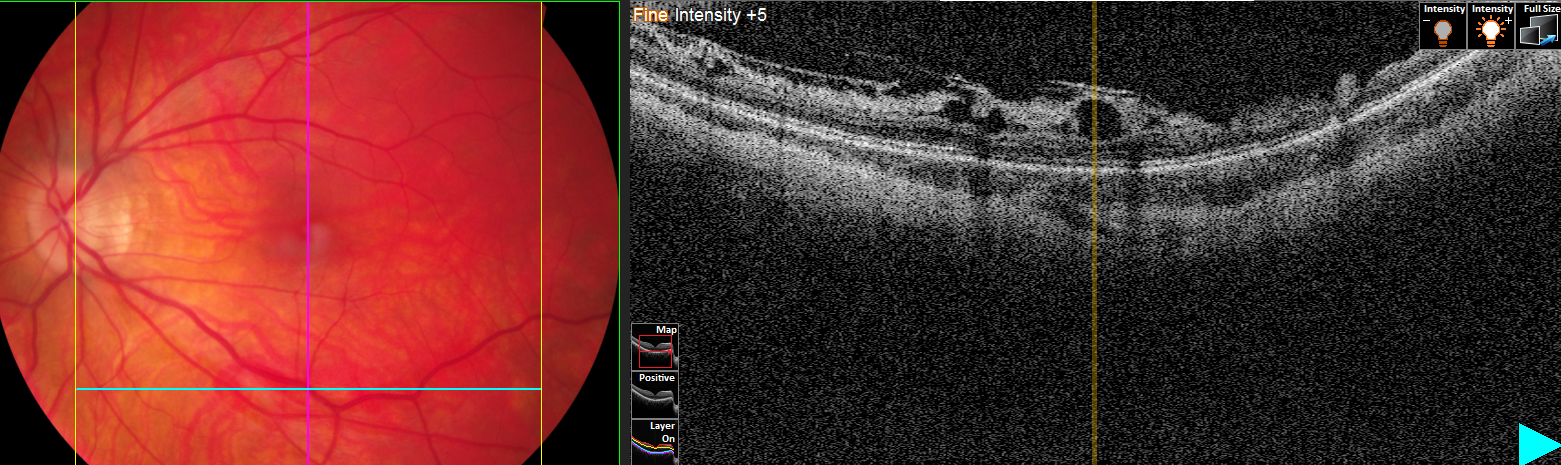
25 year old female who has had PRK for -12Rx; Her chief complaint is blurry distance vision (has to squint all the time with glare and light sensitivity).
BCVA is 20/20 with a refraction of OD -0.25-0.25×035 and OS pl-0.25×135.
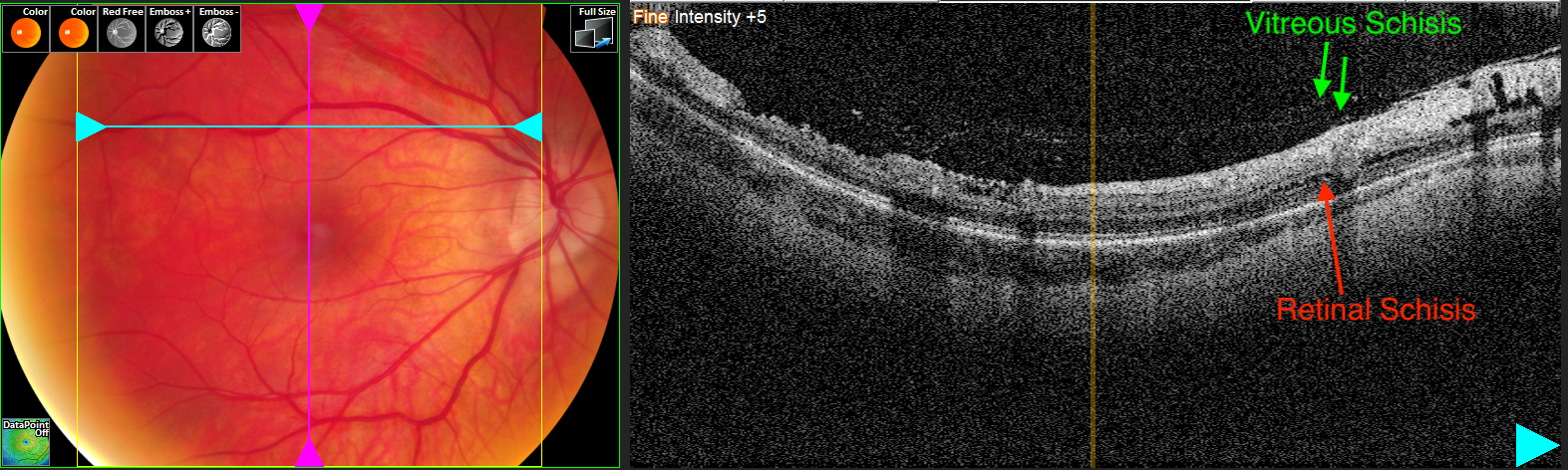
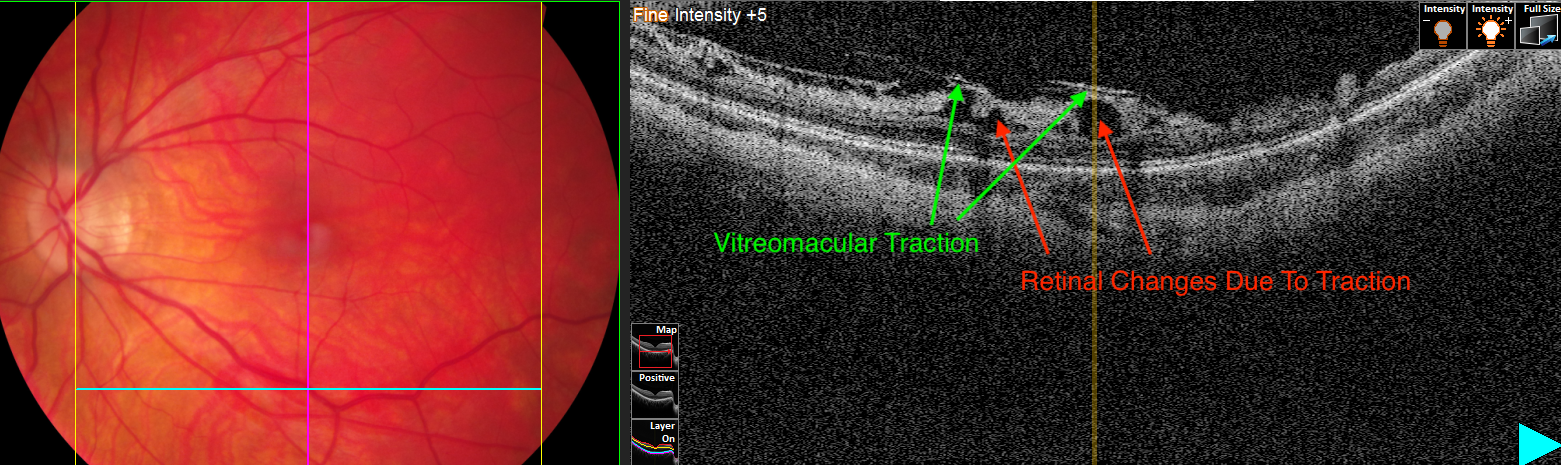
On fundus/OCT evaluation the foveal area is normal but she has an ERM OU causing para-foveal traction and what appears to be splitting in the retina.
How often do you see an ERM with traction? Do these cases warrant a referral to a retinal specialist?
Dr Lederer’s Response:
Great case! As you point out the foveal region has excellent anatomy. It is the superior and inferior macula that has the interesting pathology. Specifically you note an epiretinal membrane with retinal schisis. There is also vitreous schisis (commonly referred to as vitreoschisis). All of these findings are in keeping with a myopic fundus. I remember seeing my first case of eccentric macular schisis and pondering at how interesting it was to only see it outside the fovea. I also remember when I first learned about vitreoschisis. It seemed so obvious in retrospect but until someone told me about the pathology I was always confused by the OCT. In your case you have both!
We could debate the terminology of classifying the interface pathology as it can be challenging to know if it is a schisis in an ERM or schisis in the vitreous but this would be a rather lengthy diatribe on semantics. In general we think of an ERM causing tangential pathology and the vitreous accounting for anterior-posterior tractional pathology.
As far as monitoring goes, the key for these cases is watching the foveal center. If the retinal schisis (not to be confused with peripheral retinoschisis) does not involve the foveal center (foveoschisis) then no treatment is typically required and monitoring alone is reasonable. In terms of an ERM, again there is no involvement to the foveal center so it too can be observed. Finally, in terms of the vitreous traction (most notably in the left eye), it too is eccentric and can be observed. This is a great case to highlight many different interface pathologies and I thank you so much for sharing!
Would you like to have Dr Lederer review your OCT? Click here to learn how.