From our May 17, 2016 newsletter.
There’s much more to the retina than meets the eye. In fact, when it comes to the retina and OCTs, there are many more questions than answers — and that’s why we have an OCT lexicon that’s always evolving, trying to keep up with the latest findings.When an OCT says “subretinal lucency”…
A technical description of an OCT may note “subretinal lucency” to suggest the lack of a definitive understanding of this finding. After all, it may be just empty space or it may be fluid. Ultimately, the term “subretinal fluid” or “subretinal lucency” is often used together with a known diagnosis.Here’s an example from wet age-related macular degeneration
Subretinal fluid is common for patients with this condition. The leakage of fluid from choroidal neovascular tissue leaves little doubt as to what is in the subretinal space (i.e. it is extravasated fluid).Here’s an example from vitreomacular traction
In post-intravitreal ocriplasmin cases, the term “subretinal lucency” is used to indicate that there may be a disconnect between the RPE and photoreceptors rather than true fluid.Tip: Call it “subretinal fluid” and call it a day
As your expertise in OCT interpretation develops, you will use more descriptive terminologies for suggesting diagnoses. In the meantime, Dr. Lederer, CEO at EyeCarePD, recommends a blanket use of the term “subretinal fluid” for OCT users not ready to commit to subtle differentiations. Why? Because the most dangerous and vision-threatening aspect is subretinal fluid. If you call it subretinal fluid, ask for a second opinion and it turns out to be a benign finding, then no harm, no foul. But if you gloss over subretinal fluid by calling it an unimportant “lucency,” then you may be missing a treatable pathology — and research shows that eye care professionals don’t sleep well at night when they think they’ve missed a treatable pathology. Keep an eye out for more tips and info from EyeCarePD.A Clear Vision for Professional Development
Elevate your eye care skills with image-rich content and relevant case examples that empower you to treat patients more effectively.
Send this Newsletter to a Friend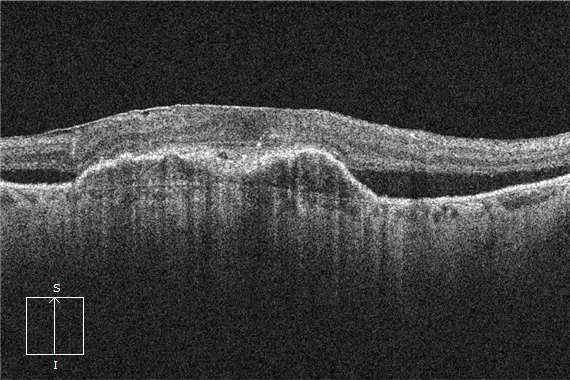

Nice tip (thumbs up) I would like to add something else on this Tip
1) Subretinal fluid is a sign of outer blood-retinal barrier defect
2) In DME the presence of Subretinal fluid may be a sign of long term clinical course and in this case if there is a poor response to AntiVEGF with absence of VMA then intravitreal steroids may be indicated
Ameen Marashi MD
Ophthalmologist-Retina Specialist
Marashi Eye Clinic
Aleppo Syria
https://www.amretina.tk