The INTERPRET: Glaucoma training software, which many of you have had a chance to play, is all about learning and practicing common skills needed to diagnose disease. However, we also all know that patients don’t read the rule book and sometimes present in atypical ways. So, we need to be ready to look past the rule book to care for such patients.
Glaucoma is a characteristic optic neuropathy. In other words, if it looks like glaucoma based on the appearance of the optic nerve, visual field (VF), and ancillary imaging parameters, then the diagnosis is glaucoma. The RNFL is one of those ancillary imaging parameters, and statistical analysis of thinning can be useful. Typically, we define patients as having suspicious thinning when their RNFL analysis falls within the 1-5% range of a normal distribution. And when the RNFL analysis falls in the <1% region (“red”), we feel much more confident in the diagnosis. But in the case below, we see something different.
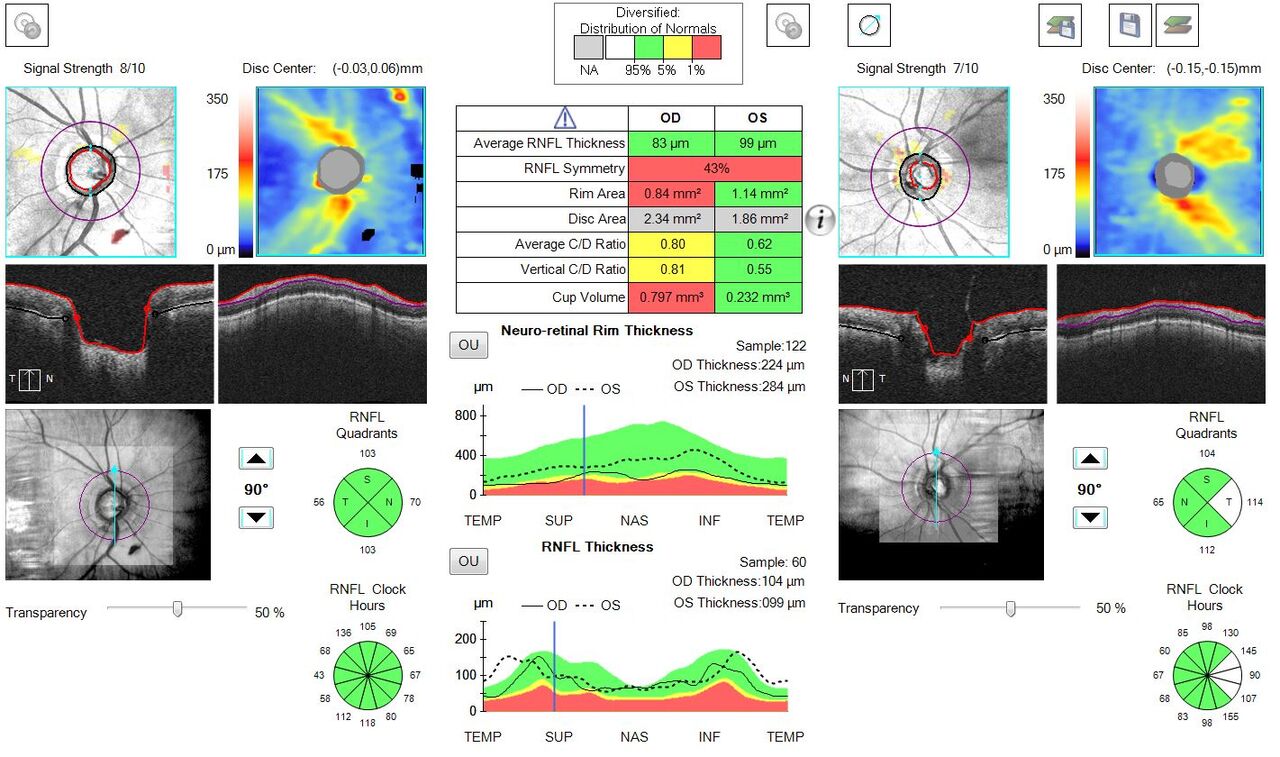
- Note the cup to disc asymmetry in the right versus the left eye.
- Note the clock hour analysis demonstrating all “green” for the right eye.
- Note the TSNIT thickness curve demonstrating relative blunting of the superior and inferior peaks OD compared with OS.
- Note the RNFL symmetry in the table is “red”, demonstrating statistically significant asymmetry between the eyes.
- Finally, note the absolute difference between the average RNFL thickness OD versus OS. There is a >10 micron difference (10 is typically used as the cutoff value when considering asymmetry).
Now here is the rub. This patient ultimately went on to a diagnosis of glaucoma based on the asymmetry between the eyes, despite the relative RNFL preservation. BUT, if the patient had both eyes present as they do in the right eye, we would have called this “normal”. Sure, we might watch carefully for progression, but if a theoretical patient had an RNFL thickness profile in both eyes exactly like that seen in the right eye of this patient, we would not call it disease!
Sure…The VF and gonioscopy and intraocular pressure and many other things are important. But isn’t it cool to delve deep into the OCT analysis? There is so much we can all learn from the OCTs of our patients.
PLAY INTERPRET NOW. IT’S FREE!
Always learning,
Dr David Lederer and The EyeCarePD Team