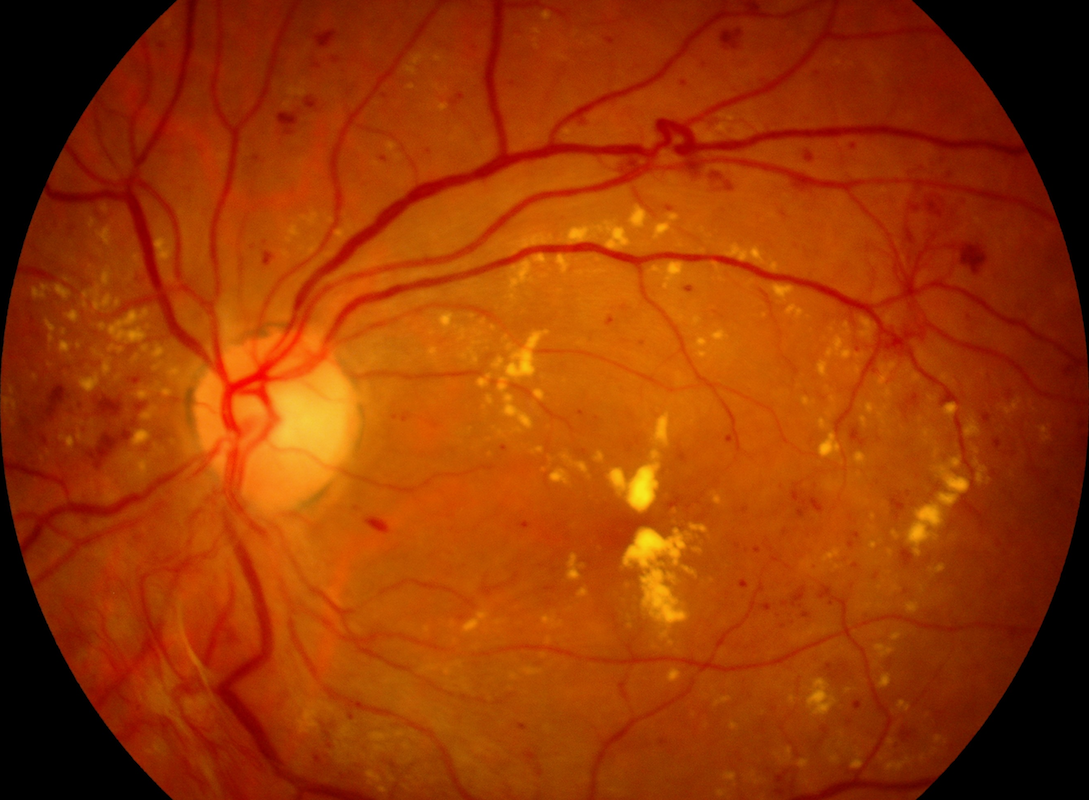
This color fundus photograph demonstrates proliferative diabetic retinopathy with clinically significant macular edema.
A Clear Vision for Professional Development
This color fundus photograph demonstrates proliferative diabetic retinopathy with clinically significant macular edema.
In this newsletter, Dr. David Lederer, CEO of EyeCarePD explains why you should use the term “subretinal fluid” first, before committing to subtle differentiations.
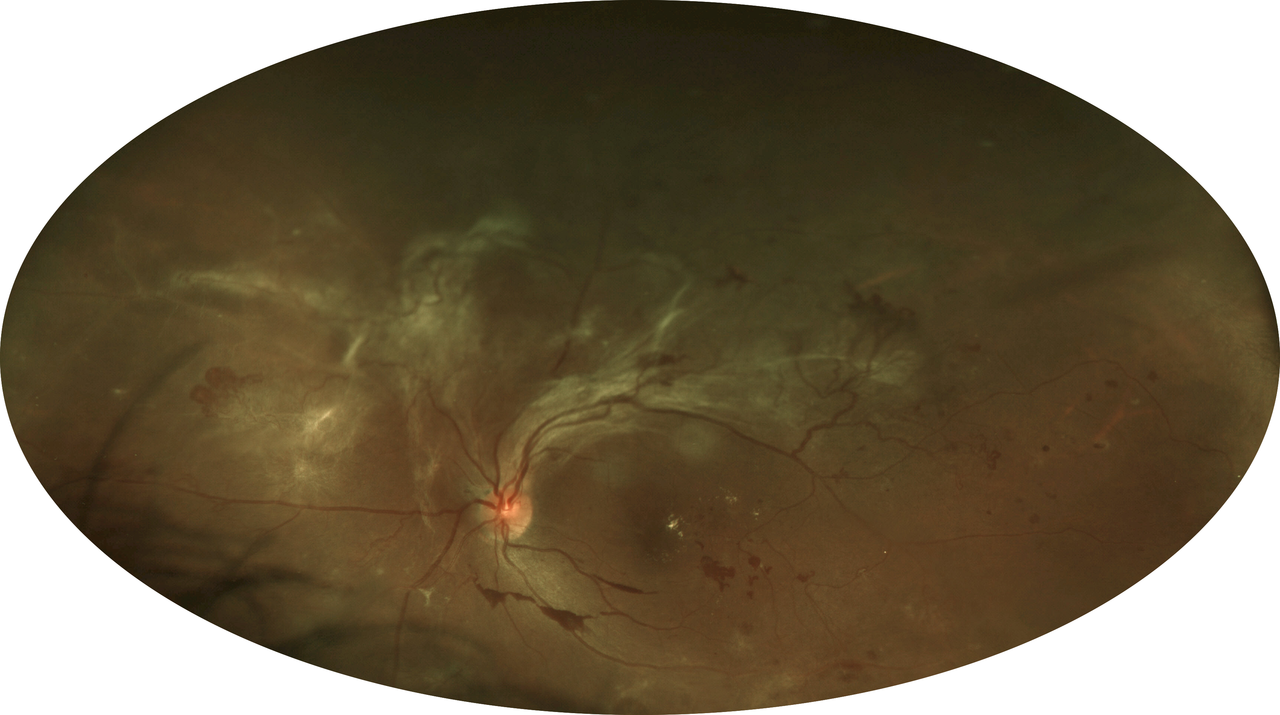
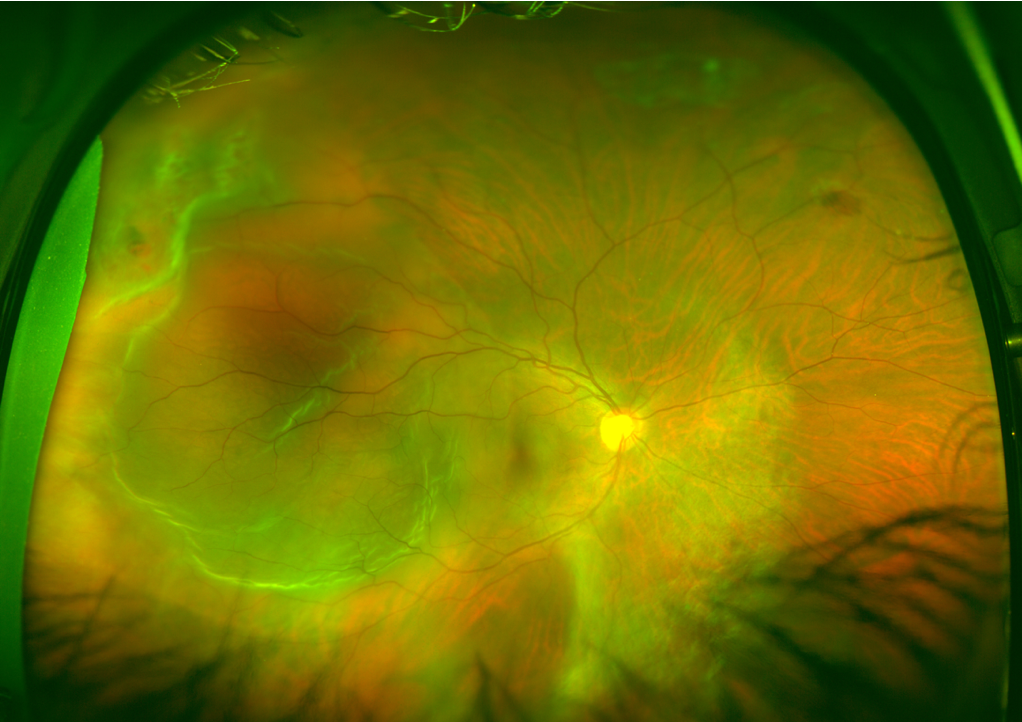
54-year-old woman who presented initially with active proliferative diabetic retinopathy and fibrotic changes.
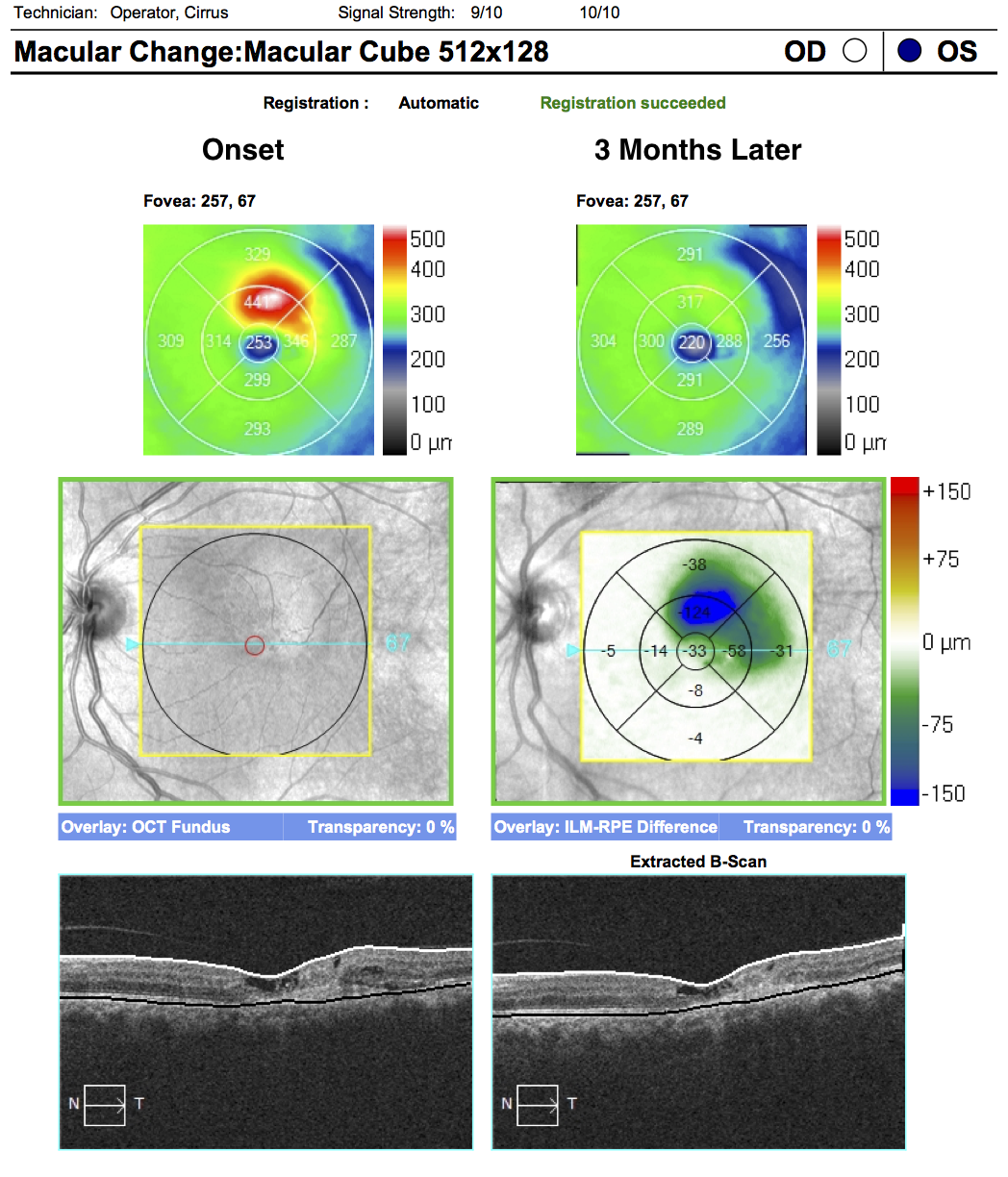
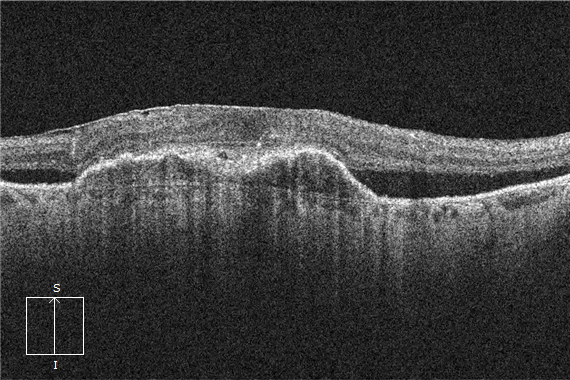
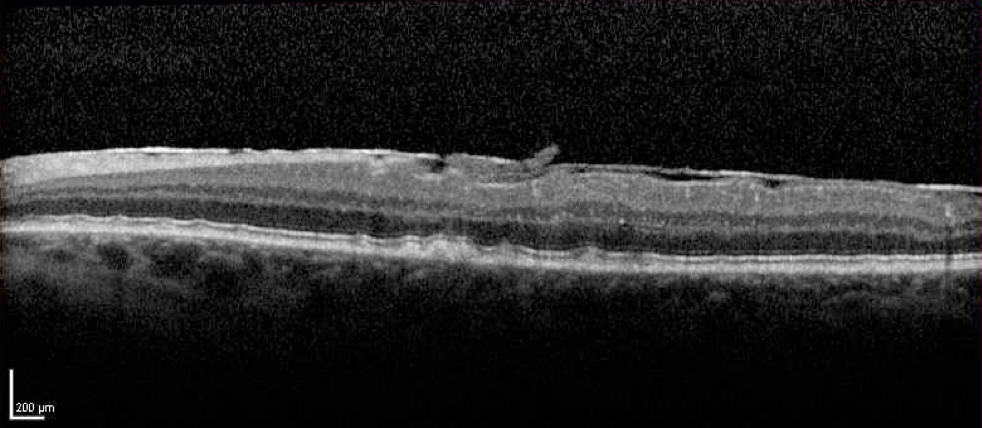
62-year-old woman with 3 monthly anti-VEGF injections. The images presented compare the presenting OCT to the follow-up OCT.
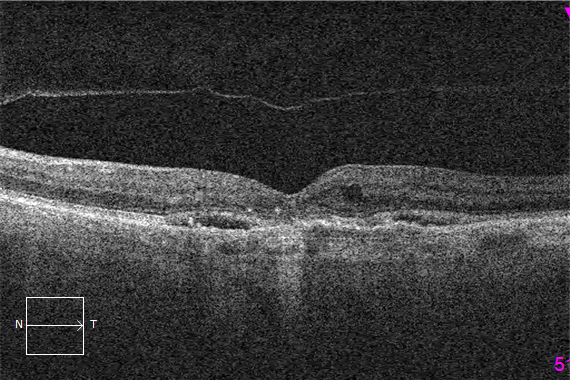
69-year-old man with Wet Age Related Macular Degeneration who is stable on quarterly anti-VEGF intravitreal injections presents for a routine follow-up evaluation.

36-year-old man with choroidal neovascularization (CNV) secondary to presumed ocular histoplasmosis.
43-year-old woman with 2 adjacent retinal breaks (red circle) and prominent subretinal fluid that involves the macula (blue circle).
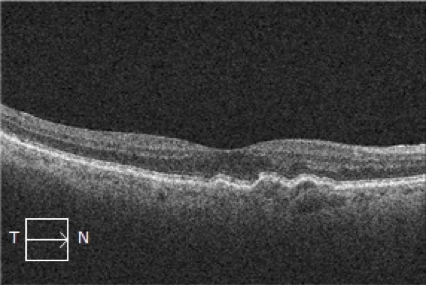
Distinguishing between the ellipsoid zone and the RPE is one of the most important steps when qualitatively evaluating an OCT.

Are you able to find the SHM and SRF?
61-year-old man with known dry AMD on routine follow-up examination.
EyeCarePD Inc.
All Rights Reserved
By using this site you agree
to our Terms and Conditions.