We’ve all seen patients with concerning presentations of macular disease. From blood to fluid, it can be confusing for the referring doctor to know how urgently a patient needs to be seen by a specialist. At EyeCarePD, we’re often asked to give advice about referral timeframes, so we’re addressing this topic here. While we do not drive policy statements, we are able to offer some guidance.
As you may have suspected, the short answer to when to refer a patient is, “it depends.” The long answer is that before you refer your patient you need a comprehensive understanding of pathophysiology, diagnosis, disease, natural history and expected outcomes. But since this isn’t always possible, here are a few things to keep in mind:
When you see a patient with blood and/or fluid in the macula…Step 1: Formulate a differential diagnosis.
- This will be based on a careful history, complete clinical examination and ancillary imaging, including OCT testing.
- Look for groupings of features on OCT images.
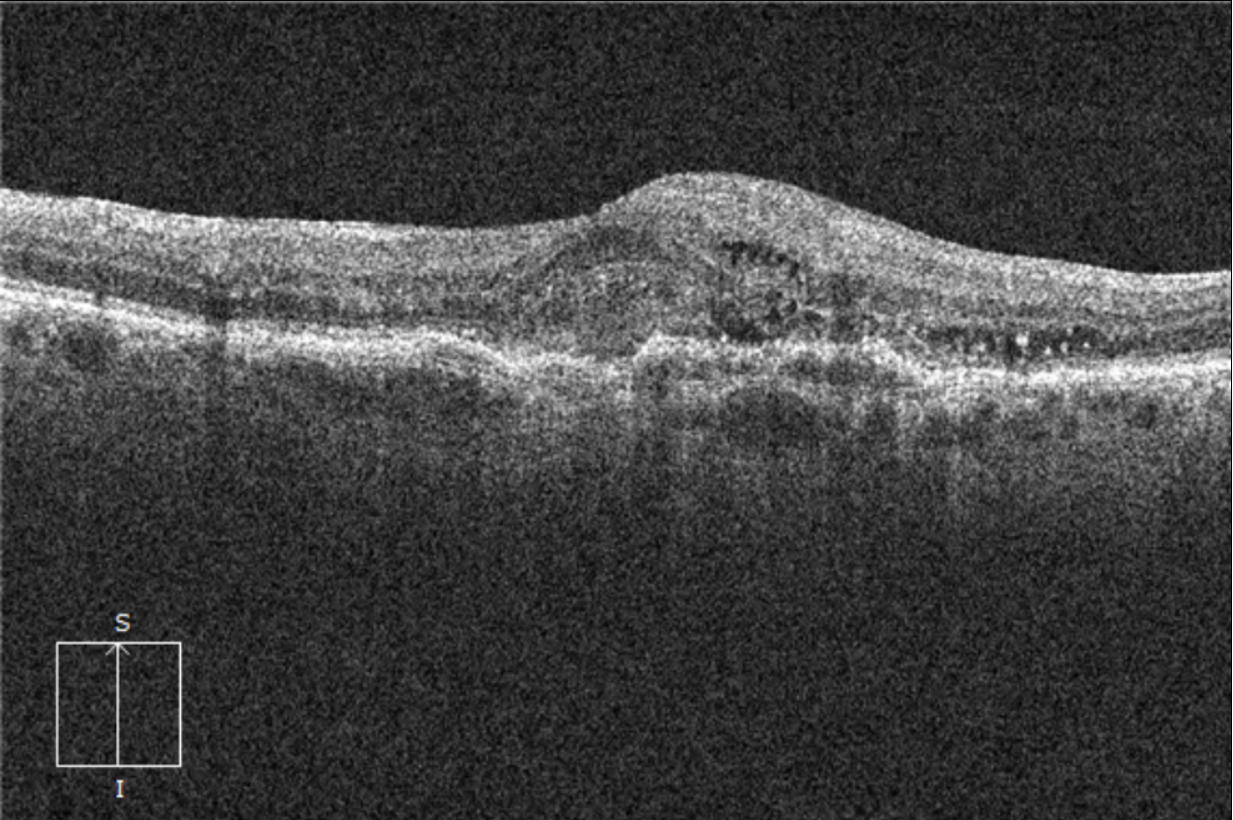
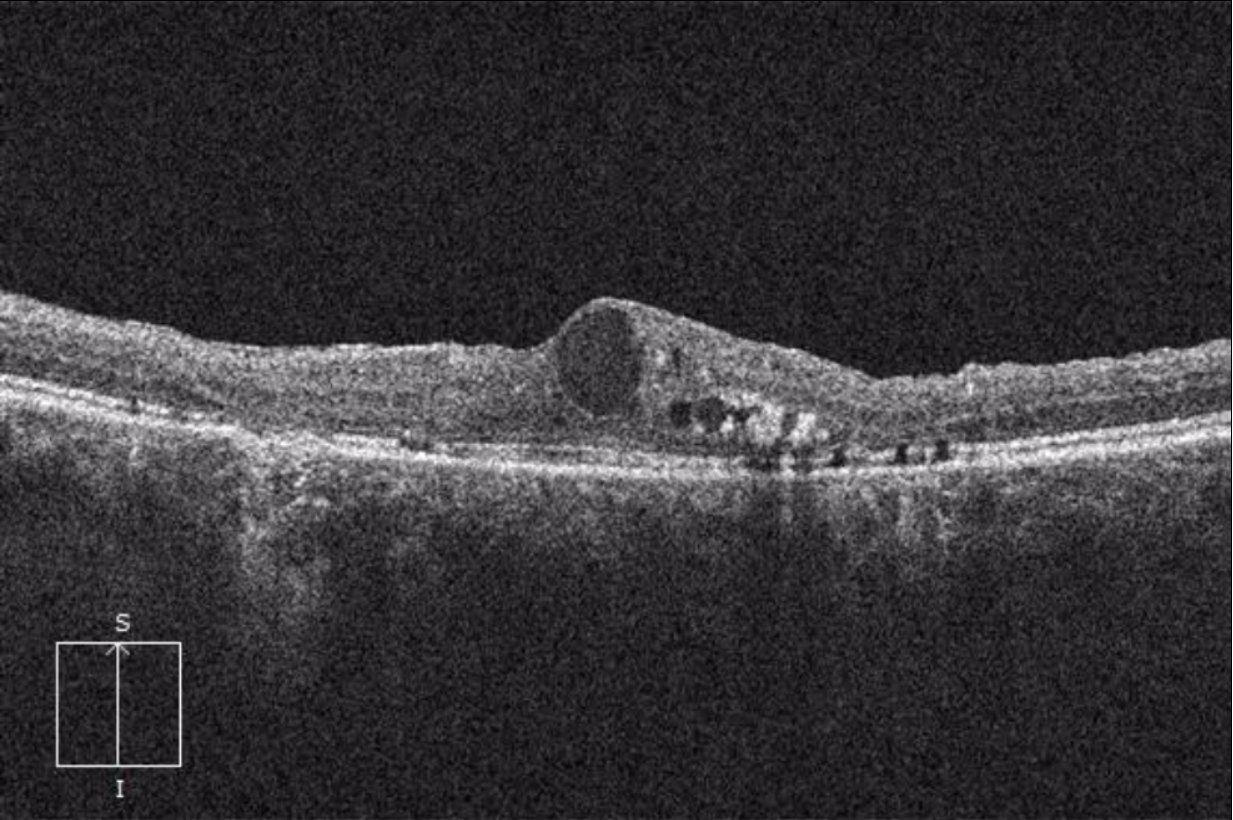
Choroidal neovascularization (CNV) often has subretinal fluid, subretinal hyperreflective material, pigment epithelial detachment and intraretinal fluid (IRF) simultaneously.
Diabetic macular edema (DME) may only display IRF with characteristic speckling and hyperreflective foci consistent with exudation.
Step 2: Remember that not all pathology is equivalent.
- CNV is due to choroidal vascular pathology, but Diabetic Retinopathy, Retinal Vein Occlusions (RVO), Postoperative Cystoid Macular Edema (CME) and Macroaneurysms are all due to retinal vascular disease.
- Additionally, acute-onset disease requires more rapid referral.
Step 3: Understand the implications of different pathologies by understanding the context of the disease.
- This includes understanding the status of the current eye and fellow eye, as well as the severity and natural history of the suspected pathology.
| PATHOLOGY | REFERRAL TIMEFRAME | COMMENTS |
|---|---|---|
| Acute-onset CNV* | Less than 2 weeks—the sooner the better | *Acute-onset presumed CNV represents an important difference from the other pathologies. Why? Because CNV has fibrotic cellular components as part of the neovascular structure. This results in fibrosis and scarring with a permanent reduction in visual acuity. Scarring can set in within days and will not resolve with anti-VEGF intravitreal therapy. |
| Chronic CNV | Within 1 month—can be longer if more chronic | |
| DME | Within 3 months | |
| Central or Branch RVO with CME | Within 1 month | |
| Macroaneurysm (with macular involvement) | Within 1 month |
So next time you’re unsure about when to refer a patient with a common macular pathology, you can refer back to this newsletter for some guidance.
Always learning,
The EyeCarePD Team
CATALOG